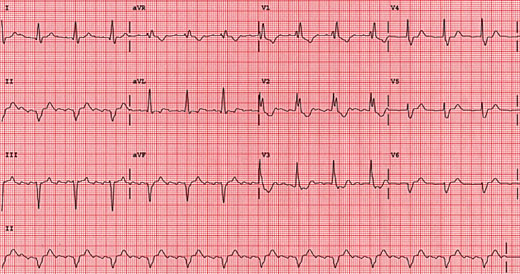
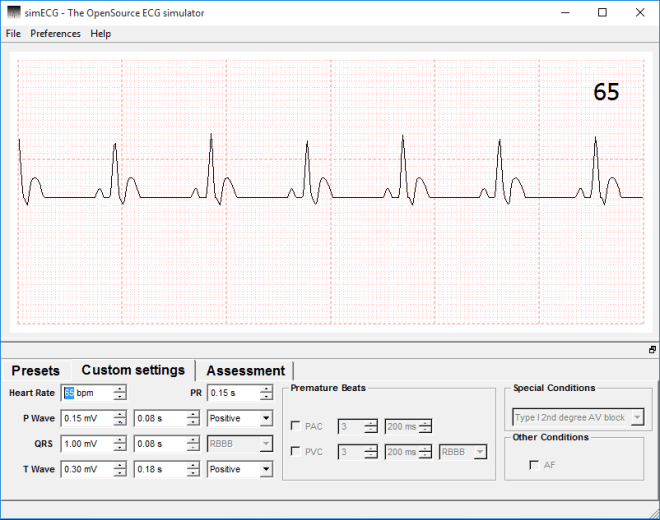
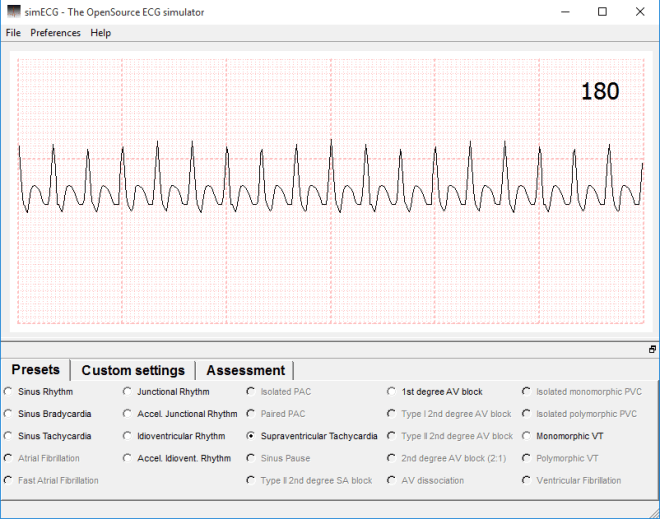
Synap is an upcoming revision tool that is driven by students. The platform enables students to create their own multiple choice questions and upload them, then download those created by others. It’s possible to “follow” other users, as you would someone on Twitter or, incidentally, this site (you can do that in the sidebar of this page…), and take any quiz that they have created. Image upload and basic editing is supported, so quizzes for physiology, such as ECG arrhythmia or echocardiography quizzes are more than possible, and are one of the reasons I decided to get involved with the whole thing. In addition, the app tracks your progress and structures your revision for you, based on your course and modules.
I’ve spent the last week or so beta testing the Synap web platform or, more specifically, I’ve been taking tests and creating basic ECG quizzes to help bug test and check functionality.
The platform, as I’ve mentioned, is currently in closed beta and only present on the web, so without having an app and a larger number of users I cannot comment on it fully, but as it stands, the processes involved in creating a profile and quiz are incredibly simple; adding and annotating images is a cinch, and a complete question only requires the user to add a correct answer and a few wrong ones. Whilst I encountered a few bugs initially, the feedback I provided was swiftly taken on board and the problems were remedied overnight. Taking quizzes is incredibly simple, and all you need to do is click “take quiz” (shockingly), then select your answers and have them marked. You can take these as many times as you like, too, and if the creator has provided any, feedback will be available for each individual question.
My only concern is the reliance on the quiz-maker supplying the correct information. I’ve taken a quiz wherein the correct answer was the only one that was possible to be correct (think “What has tusks and a trunk? 1) Elephant 2)Belephant 3)Your hamster”) yet I was still told my answer was wrong. This is a closed beta, though and that’s what these processes are for. I know it hasn’t escaped the attention of the developers, so we shall see how it is dealt with.
To break all of this down and show you what I know for sure so far, have a look at this (incomplete) features list:
- MCQs:
- Image/annotation upload
- Correct answer & up to 5 incorrect
- Optional feedback for test-taker
- Optional link to external learning resource
- Test result calculation
- Obtainable achievements
- Personalised revision quizzes sent to you
- Community links based on:
- Course/Discipline
- Cohort
- Institution
I’ll add to this list the more familiar I become with the platform.
Omair and James, its creators, and the rest of the Synap team hope that this app will enable students nationwide to help each other and revise together, and it’s a pleasure for me to be involved, even if it’s only in a small way, currently. I’ll continue to post updates as things progress.
For more info, visit @Synap on twitter.
Thanks