Myself and some of my colleagues recently relinquished a Saturday off, and braved the icy cold (read: British) weather to try to meet with the public, and raise awareness of atrial fibrillation through a project spearheaded by the AF Association.
I didn’t organise the event, but was kindly invited along, and jumped at the chance to help some of my amazing Cardiology workmates by checking pulses, and recording rhythm strips using the AliveCor mobile ECG monitor (which I have previously reviewed here).
AF is an atrial arrhythmia, wherein the sinus node does not cause appropriate, rhythmic depolarisation as it normally would. Rather, multiple foci activate, facilitating a motion akin to ‘quivering’, which raises the risk of embolism through the inefficient pushing of the blood into the ventricles. It’s an incredibly dangerous problem if left untreated, so it’s vital that it gets detected, and preferably this would happen early.

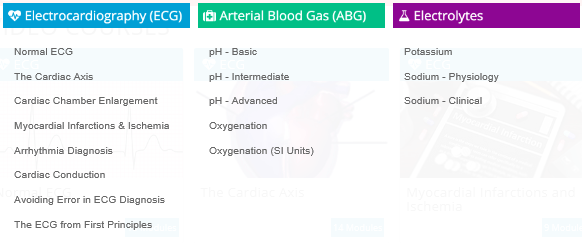
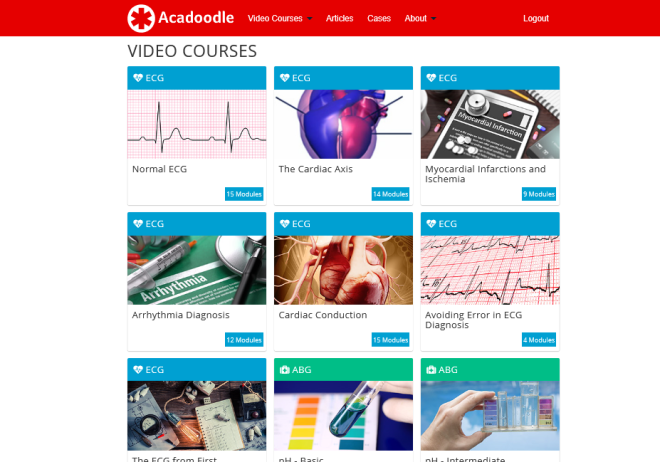
I go into detail about AF, it’s mechanisms and ECG presentation in this study guide, so have a look at that if you want to understand it further.
As you may or may not be aware, atrial fibrillation is, globally, the most common clinically significant cardiac arrhythmia, and it is thought that whilst 1.2 million people (a conservative estimate) in the UK are known sufferers of the sinus node disorder, a 500,000 have it, and live undiagnosed. The estimated cost of AF to the NHS was somewhere in region of £2.2 billion, in 2008, and given that the prevalence of the arrhythmia has increased year on year, this number may well be higher now.
Obviously, this is far from an exhaustive exploration of AF, but hopefully it gives some insight into why it’s so important to detect and treat, and why initiatives such as this one are a good idea.
We set up shop in Frome’s Westaway shopping centre at around 10am, where members of the public who’d read about the event in the local newspaper were already queueing. We four clinical scientists proceeded to advise and check 85 people throughout the day. We had a surprise visit from Cardiologist’s Kitchen, too!

Many people we talked to had little-to-no idea what the condition was, its risks, or how it was treated, so we used literature, ECG examples, and a scale model of a heart, to educate, and taught people how to check their own pulse before performing quick rhythm recordings which we analysed on the spot. More than a few people who attended had known AF, and their questions largely involved their current treatment, and the potential impact AF might have on their life. Most, however, visited so they could get checked over, hopefully putting their mind at rest, and learning something in the process.
We didn’t find any new atrial fibrillation (although we did discover two cases of previously undiscovered AV Block), but of equal importance to arrhythmia discovery, was the community engagement, particularly in a public setting. In clinics it’s easy to fall into a cycle with patients, due to schedules and time pressures, and whilst we all try our hardest to make sure everyone is treated individually, seeing the problem before the person is always possible. Interacting with patients on “their turf” meant the ball was in their court, if you like, and the sheer volume of people who expressed an interest meant it couldn’t have been further from a wasted day.
The feedback we received was overwhelmingly positive, and there was a recurring theme in the gratitude people felt for the healthcare environment coming to them, as oppose to the other way around. Many of those to whom we chatted understand the strain that hospitals and GP surgeries are under, and felt that visiting to be checked for AF, and other such things, would be inappropriate. In many ways, I suppose they’re right, too; regardless of the importance of finding these things, especially as they do not always present with obvious symptoms, healthcare centres, unfortunately, cannot cope with the demand a service such as this would present. To this end, I was glad to have ventured out to participate in this, an outdoor clinic of sorts, and educate the public on what to look for, as well as how they can guage their own heart rhythm and take some more control over their own health. I sincerely hope to do it again soon!

The AFA is a fantastic charity, so it’d be great if you were to find out a bit more about them by visiting them here.
I’d like to thank my colleagues for asking me to participate, and generally being fantastic people, those who visited us and asked lots of challenging questions, and the kind souls who bought us ginger ale and flapjacks when the temperature reached what *felt* like sub-zero levels.
The statistics used in this post are taken from the BHF. If you want to take a look for yourself, visit the British Heart Foundation, here.