Myself and OliGS recently sat the SCST Electrocardiography Diploma and Practical Examination, so I thought I’d jot down some of my experiences in the run up, and my retrospective thoughts on the day itself.
If you’re thinking of doing it, or have your PTP finals looming, then read on, as this will give you an idea of what to expect.
I’ll start by saying this: Oli and I have NEVER been so stressed in our entire lives.
This exam was a nightmare for which to prepare; I have extensive experience in taking exams, and it is my view that they’re 50% what you know, and 50% what the examiners want you to tell them. Without having met these examiners or seen a previous paper, it was very difficult to know what to really nail, in the revision stage. The syllabus was long, detailed, and contained what seemed like an entire career’s-worth of things to learn, so we already knew it was going to be a slog, but nothing prepared us for the written paper…
Read these. Lots.
We studied, sometimes sleeplessly, for weeks. Tested each other on rare arrhythmias, read textbooks cover-to-cover (repeatedly), and watched each other’s once sunny outlooks and youthful (ahem) features rapidly wither as the examination date draw closer. It consisted of 20 multiple choice questions, 10 arrhythmia analysis and knowledge questions, and 4 full ECG analysis recordings. Some of these were almost instantly recognisable, but others were brutally difficult to analyse. The MCQs (often the most looked-forward to section of any exam) were equally tough. Those 3 hours lasted a lifetime…
We left the exam battered and bruised, but glad it was over.
But it wasn’t over. It was far from over. As well as the written paper that had almost ruined us, we had the practical exam to do as well.
We had made sure that during our post-ECG placements we still got ourselves in the clinic so as to keep everything fresh, as performing a perfect ECG is not like riding a bicycle.
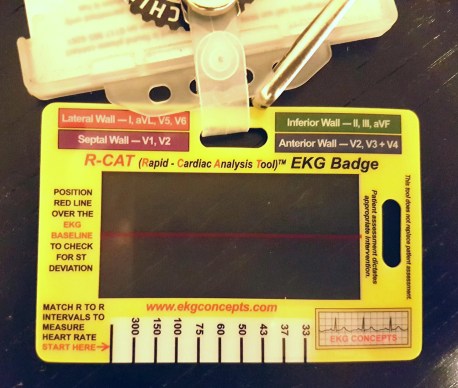
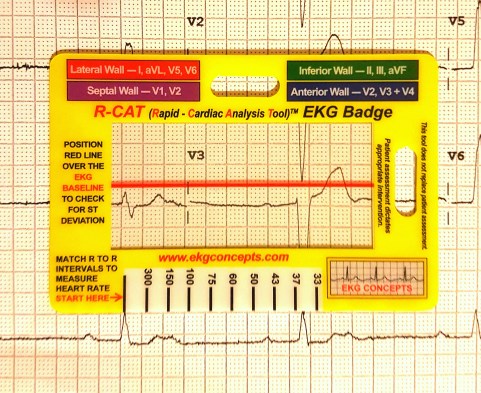
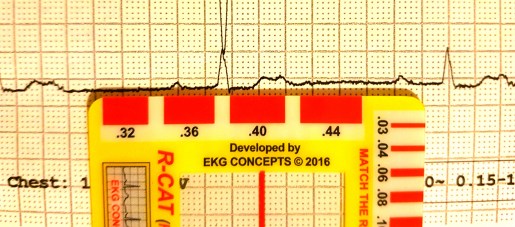
The last attempt before test day
It turns out that this was the correct call, as was practicing on one another in the hotel the evening before the exam; the margin for error in the exam is 2mm(!) Anyone who’s had an informal assessment, or had their Direct Observed Practice scrutinised whilst training knows that it’s very easy to second-guess when it comes to electrode placement, and despite having 20 minutes to complete the whole thing, this timeframe becomes devastatingly short once you’re in there. It’s a clinical assessment, so one needs to complete the necessary ID checks, explain the procedure to the patient AND to the examiners (i.e. in two different ways), perform it whist answering questions, and then complete a verbal examination.
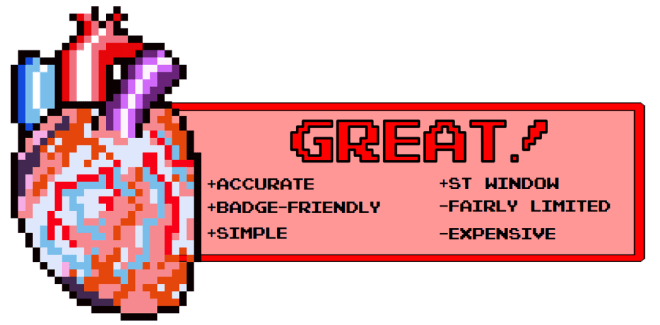
Three hours after we had finished the written paper, we were called to attempt our practical exam. There were ashen faces all around. Some were on those still waiting for their number to be called as ours had just been, others had been told that their 2 attempts had been unsuccessful. Neither of us were looking forward to this. Now, given that I’ve already stated that each electrode is allowed to deviate only 2mm from the precise, gold standard location, the internet-purchased electrodes pictured in the above image would be somewhat unfair, right? It seems that the examination board concur, as they provide some rather cool, transparent electrodes complete with crosshairs. They doesn’t make it easier, per se, but they certainly go some way eliminate that lingering trepidation when it comes to deciding you’re happy with your placement and ready for judgement.
Crosshair emblazoned electrodes(!)
I opted for the “all at once” technique: I explained everything to the patient before I started, gained consent, then explained everything I was doing as I went along. Once was put simply to the patient, then once to the examiners, using correct terminology. I paid extra special attention to V1, V2 and V4, as my patient had a particularly wide sternum, so I wanted to be totally sure that I had the sternal border, especially given the electrodes were rather far apart when placed and looked slightly odd to me. After I took a step back and looked at my work, I was incredibly tempted to move the aforementioned electrodes, but either due to fear, fatigue, or a combination of the two, I decided to leave them as they were, opting to go with my initial judgement. After that, I waited.
I’m not entirely sure how the placements are measured, as candidates are asked to leave the room whilst they are checked by two examiners. I heard someone mentioning special rulers, but I didn’t get a look at them (it’s all very cloak and dagger), in any event, you’re called back into the room and, in my case at least, informed of your passing or failing grade. I’m pleased to report that I passed on the first attempt, which as I’m sure you can imagine, was a tremendous relief; I lost my cool somewhat, and expressed my joy rather loudly, as I was informed I wouldn’t have to do it again. Oli soon found me in the waiting area and, grinning wildly, slapped me on the back and hissed “YESSSSS!” before promptly throwing himself into a chair. It was over, and we were victorious.
We didn’t speak too much about it, on the way home, but in the couple of days that have passed since the exam, we both feel a tremendous sense of pride that we actually did it, and did it successfully. If I were to give you all some advice, it would be the following:
- Be prepared for anything and everything, including waiting around for a long while
- Practice analysing ECGs until you hate them
- Practice performing ECGs until you hate them
- Go with your gut as much as you can during the practical exam
- Bring lunch
- Don’t under ANY circumstances, stay at the Ibis Hotel in Birmingham’s Chinatown district (I can’t stress this enough because it backs onto a nightclub that doesn’t stop playing the most bass-heavy music until the wee hours of the morning)