The fact that this specialist degree exists primarily in universities is a relatively new event; before the shakeup by Modernising Scientific Careers, the majority of training was completed in-house with an element of distance learning thrown in to assist with the theory behind the practical concepts.
As physiological science makes the transition to a 100% university- led discipline, there remain students that are still learning the “old way”. Sarah is one of those people, and I had the pleasure of working with her this year during my rotations between respiratory medicine and cardiology. In order to get a bit of insight into exactly how the course differs between bases, she kindly agreed to be interviewed for TSP.

Hello Sarah! Could you outline the structure of your week, with regards to working in your department and studying the degree simultaneously?
I’m employed by the hospital, so have to work my set hours which are Monday – Friday 08.30-16.30. Although I’m studying, I am not employed as a student, rather, I am an Assistant Technical Officer, which basically means I help around the department doing admin, portering and some clinical work. I have certain responsibilities with regards to admin that I have to keep on top of regardless of what clinical work I need to be learning.
Monday is my main admin day, so I spend the entire day sorting through referrals, checking messages & booking appointments for certain procedures that only I book. I need to keep on top of this as some of the procedures have extremely long waiting lists, so if a patient cancels last minute I need to try my best to fill that slot. Once my admin is complete I normally help out my colleague in the office with some of her work load. If there is no porter to bring inpatients up & back for echocardiograms then it is part of my job to do this as well, which means I can’t get my necessary admin work completed.
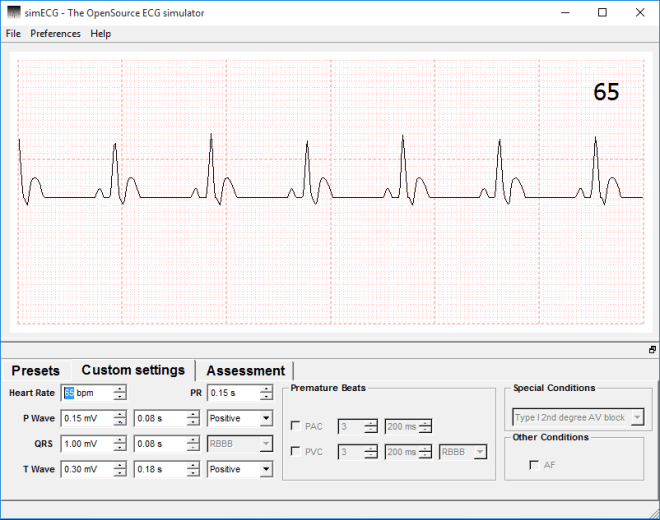
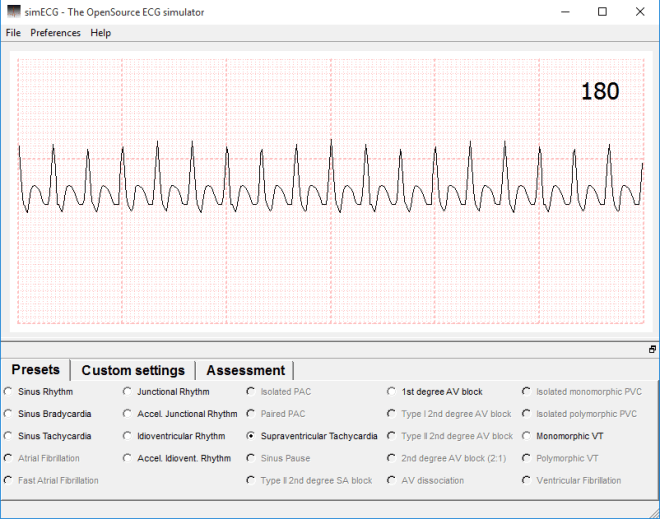
Tuesday is the start of my clinical week, unless I have been portering the previous day. At the moment I am spending all day Tuesday in analysis, analysing 24 hour and 48 hour tapes. I am able to analyse a tape independently, but as I am still learning they all need to be checked after, just in case I’ve missed something or worded my report incorrectly.
Wednesday is a half day in the department for me as I have a collaborate session starting at 12.00 so I need to be set up in the library ready to start. After my collaborate session I catch up on any studying I need to do, such as looking over lectures that have been released for the following week, researching/ writing an assignment or revising for upcoming exams. On a Wednesday morning I will either be fitting ambulatory blood pressure monitors (supervised, as I am not confident to do them alone yet) or analysing.
Thursday mornings I am in Electrocardiography, either in the department or going down to the ward, and in the afternoon I analyse.
Friday mornings I do tape clinic which occupies the entire morning and keeps me very busy, especially if I have patients returning that have had symptoms of dizziness & I need to get the tapes checked before I can let them go. I spend Friday afternoons in analysis.
That is my current working week, but I will start going on the rota soon to sit in on exercise treadmill tests as well. Most mornings I get into work at around 07.30 so I can get some studying done before work and I try to do an hour or so in the evening as well. Most weekends I keep to myself, but if I have an assignment due or exams I will do a couple of hours each day.
That’s a hectic week. This might now be a silly question, but do you feel that this is this enough?
In terms of clinical exposure … yes! But it is very hard to keep up with the academic work load when there is very little time to fit things in. I commute for over 2 hours a day so this eats into my potential study time, but I try to keep a balance of work, study and actually having a life!
Do you feel that working in the same department as you study helps you to learn more and keep you motivated?
I feel that second year especially has helped me learn, but most of the academic work in our first year wasn’t particularly relevant to cardiology. I feel like I learnt more in the last 2 months from analysing tapes than I have in the whole 2 years that I’ve worked in the department. I definitely think it has helped to keep me motivated as I’m constantly surrounded by people that are doing the job I am training for, so I’ve got a clear goal at the end of it.
You’re one of the last sets of the distance intake. Do you think, if you had the choice, you’d still do the degree in the manner you currently are, or would you choose to be based at the university?
I’ve already done a previous degree so I’ve experienced the whole student life thing, so I’m not missing out by doing it this way. At the moment I am essentially being paid to learn, which is ideal. I wouldn’t be able to afford to do this degree if I was based at the university, as I’ve already had a student loan so I’m not entitled to another. I think I get a good amount of exposure in the clinical setting, but I just have to do some of the boring admin jobs to make up for it. At the end of my degree I will have a job and I know 100% that this is the career I want for myself. I wasn’t passionate about my previous degree subject so I lost interest and didn’t want to spend the rest of my life doing it, whereas I know from working in this department and from studying the way I am, that this is what I want to do. I don’t think I’d have that level of clarity if I was based more at the university than the hospital.
That’s fair. When we worked together during my placement, I was aware of the fact that you were much more comfortable in the clinic environment than I was (obviously), so what do you feel we at the university have by way of an advantage?
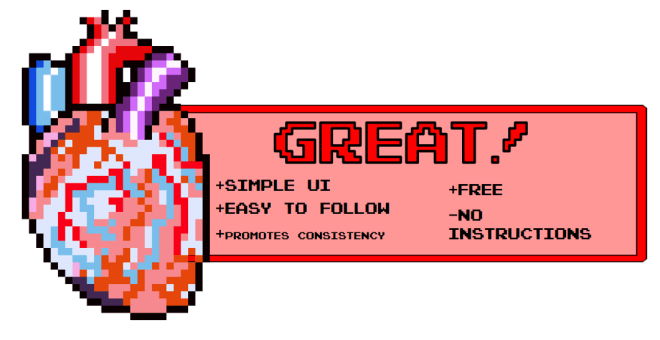
I definitely think that as I’m exposed to patients and the environment all day every day that I am more confident and comfortable than yourself, but I would say that full time students based at the university have a lot more academic knowledge. We have 1/2 hours a week of contact time with our lecturers so we need to go out and research ourselves, whereas it is clear that you guys have a lot more academic time although you miss out a lot with the lack of placement.
Thanks, Sarah!
As you can probably tell, despite the fact that Sarah and myself are in the same cohort, our academic years have a vastly different focus. As I (rightly) assumed just from working with her on the department, both routes present their pros and cons, and seeing as this is a vastly understaffed form of diagnostic science, it does, in my opinion, open the career up to a greater number of people now it will be university- led.
If you’ve got an opinion, or a question regarding anything you’ve read, sound off in the comments below.
Photo courtesy of Facebook